Rare Case of Yersinia Enterocolitica Causing Infection of a Temporal Venolymphatic Malformation
Phillip Cantwell*, Shahriar Raj Zaman, Jeremy Rawlins
Department of Plastic Surgery, Royal Perth Hospital, Australia
*Corresponding author: Phillip Cantwell, Department of Plastic Surgery, Royal Perth Hospital, Australia. Email: pcc998@uowmail.edu.au
Citation: Cantwell P, Zaman SR, Rawlins J (2020) Rare Case of Yersinia Enterocolitica Causing Infection of a Temporal Venolymphatic Malformation. Annal Cas Rep Rev: ACRR-108.
Received Date: 01 April, 2020; Accepted Date: 07 April, 2020; Published Date: 13 April, 2020
Abstract
Described is the case of a 29-year-old male with Y. enterocolitica subclinical colitis causing an infected venolymphatic malformation, presenting as a large septic left temporal swelling. The patient was given IV antibiotics and over the course of a week the swelling significantly decreased in size and the patient’s diarrhoea subsided; thus, the decision was made to not operate. Most extraintestinal case reports of Y. enterocolitica occur in immunosuppressed patients. Our case demonstrates a situation where even a young and healthy individual can develop seeding sepsis outside of the intestinal tract.
Clinical record
A 29-year-old male with no past medical history presented to the emergency department with a 2-day history of left temporal swelling, fever and intermittent diarrhoea for several weeks in the lead-up. Upon examination, the patient had a temperature of 38.4°C, a heart rate of 120 BPM, a non-tender abdomen, and a large swelling in his left temporal region. Blood was taken, which demonstrated an elevated white cell count of 12.5×109/L and a C-reactive protein of 160mg/L. Blood cultures taken at that time later grew Yersinia enterocolitica. As the patient was stable, an MRI was performed to characterise the swelling in his left temporal region (Figure 1), which showed an infected venolymphatic malformation.
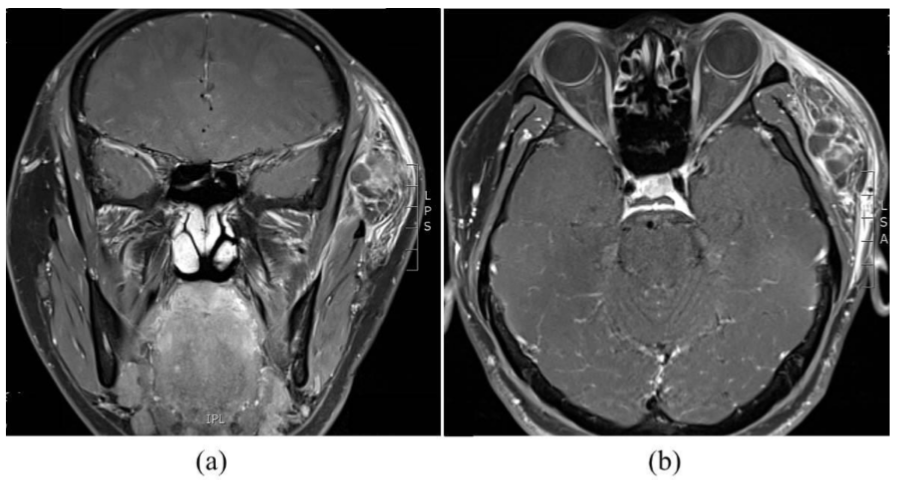
Figure 1: MRI images of the patient on admission (a) coronal view; (b) axial view.
The patient was given IV antibiotics; initially cephazolin, which was changed to cefepime on the advice of the Infectious Diseases team when blood culture results were made available. During the course of a week, the swelling significantly decreased in size and the patient’s diarrhoea subsided; thus, the decision was made to not operate. The patient was discharged home on a 3-week course of oral antibiotics (ciprofloxacin) with clinic follow up.
At the one-month review, the left temporal swelling was no longer noticeable, and repeat MRI showed a significant decrease in swelling (Figure 2).
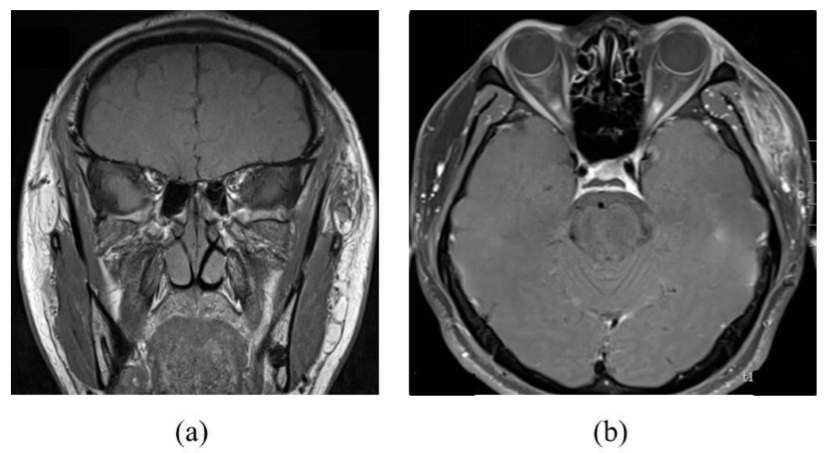
Figure 2: MRI images of the patient one month after discharge from hospital (a) coronal view; (b) axial view
Discussion
This case demonstrates an extraintestinal manifestation of Yersinia enterocolitica. The diagnosis was confirmed with a positive blood culture in conjunction with MRI findings of the infected left temporal venolymphatic malformation. Upon introduction of the appropriate antibiotics (cefepime), both fever and swelling were reduced, supporting the diagnosis. The infected site did not undergo fine needle aspiration or drainage given the confidence in diagnosis and risk to the patient associated with both of these procedures.
Yersinia enterocolitica is a gram-negative bacterial species in the family enterobacteriaceae, most commonly causing gastrointestinal infections, such as enteritis and pseudoappendicular syndrome [1]. Most cases of Y. enterocolitica self-resolve without requiring antibiotics [2], with transmission occurring zoonotically or via the consumption of contaminated foods (i.e., via contaminated food, water, or milk) [2,3]. Although rare, there have been case reports of person-to-person transmission [3].
After ingestion, Y. enterocolitica has a predilection for the terminal ileum, where the bacteria are able to penetrate M cells within Peyer’s patches [3]. This typically leads to the presentation of fever, diarrhoea, and abdominal pain approximately one week after exposure [3].
Iron is considered to be an essential growth factor for bacteria; therefore, patients with iron overload are at higher risk of Y. Enterocolitica extraintestinal disease [3].
The majority of Y. enterocolitica infections occur sporadically with the sources unknown, however large outbreaks have previously been reported [3]. Most infections are self-limiting and do not require antibiotics, with therapy indicated for patients with septicaemia, focal extraintestinal infection, or who are immunocompromised [3]. The mortality rates of patients with Y. Enterocolitica septicaemia is 7.5% [4].
Extraintestinal manifestations of Y. enterocolitica are uncommon [1], however case reports involving infection of aneurysms, the respiratory system, and the skeletal system have been reported [1,2]. No known cases of Y. enterocolitica causing infected vascular malformations have been identified in the literature. We present a case of Y. enterocolitica subclinical colitis causing an infected venolymphatic malformation and presenting as a large septic left temporal swelling.
Most extraintestinal case reports of Y. enterocolitica occur in immunosuppressed patients [2]. Our case demonstrates a situation where even a young and healthy individual can develop seeding sepsis outside of the intestinal tract. Thus, heightened clinical investigation and historical examination are recommended to contribute to the knowledge base and the advancement of best practice.
Lessons
Yersinia enterocolitica is a gram-negative bacterial species in the family enterobacteriaceae, most commonly causing gastrointestinal infections, such as enteritis and pseudoappendicular syndrome.
Most extraintestinal manifestations of Yersinia enterocolitica occur in immunosuppressed patients. The majority of Yersinia enterocolitica infections occur sporadically with the sources unknown, however large outbreaks have previously been reported.
With appropriate response, antibiotic therapy may be a valid alternative for treatment in patients with infectious collections where drainage may put patients at high morbidity risk.
References
- Hagensee M (1994) Mycotic aortic aneurysm due to Yersinia enterocolitica. Clinical Infectious Diseases 19: 801-802.
- Mofredj A, Guerin JM, Leibinger F, Masmoudi R (2003) Spontaneous Pleural Empyema due to Yersinia enterocolitica. Southern Medical Journal 96: 525-527.
- Watanabe K, Watanabe N, Jin M, Matsuhashi T, Koizumi S, et al. (2014) Mesenteric lymph node abscess sue to Yersinia enterocolitica: case report and review of the literature. Clinical Journal of Gastroenterology 7: 41-47.
- Gayraud M, Scavizzi M, Mollaret H, Guillevin L, Hornstein M (1993) Antibiotic treatment of Yersinia enterocolitica septicaemia: a retrospective review of 43 cases. Clinical Infectious Diseases 17: 405-419.
